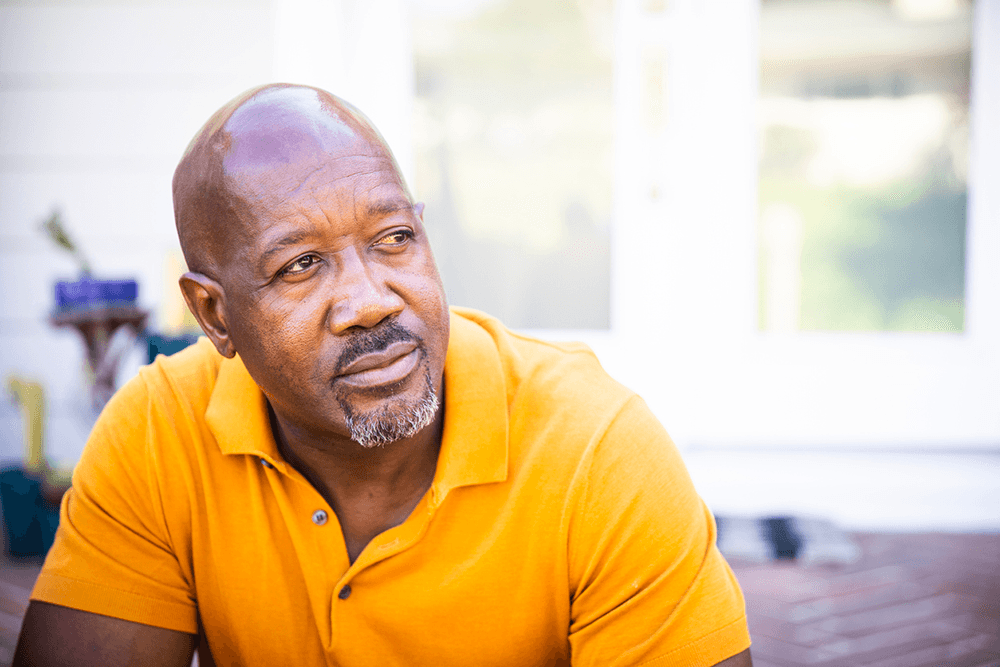
Unclassifiable ILD
OVERVIEW
- Even after extensive clinical, radiologic, and/or pathologic examination physicians may still be unable to classify a patient's idiopathic interstitial pneumonia (IIP)1
- In these cases, the pulmonologist should determine the best course of treatment based on the most probable diagnosis after a detailed discussion with the pathologist and radiologist1
This category designation should not be used for cases in which the distinction between the usual interstitial pneumonia (UIP) and fibrosing nonspecific interstitial pneumonia (NSIP) patterns is difficult.1
Most common reasons for an unclassifiable diagnosis are conflicting data or lack thereof.2
- 10% of all ILDs are considered unclassifiable2
FIVE MAIN REASONS FOR AN “UNCLASSIFIABLE” DIAGNOSIS2
- Conflicting clinical/radiologic/histopathologic data
- No biopsy: high surgical risk
- No biopsy: mild/stable disease
- No biopsy: unwillingness of patient
- Insufficient tissue on biopsy
EPIDEMIOLOGY
SURVIVAL AND MORTALITY2
Survival
- >50% 5-year survival rate
- 20% better survival than patients with IPF
Predictors of Mortality
- DLCO <35%
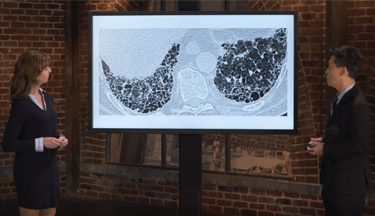
- High fibrosis score on HRCT
- Former smoker
See also
Test your knowledge

Bridging Educational Gaps in ILD
Media Library